Dyslipidemia, zaburzenie metabolizmu lipidów, stanowi globalny problem zdrowotny. Dyslipidemia jest ściśle związana z rozwojem chorób układu krążenia, które są jedną z najczęstszych przyczyn zgonów. Podwyższony poziom cholesterolu, zwłaszcza cholesterolu LDL, może przyczyniać się do tworzenia blaszek miażdżycowych w naczyniach krwionośnych oraz zawałów serca i udarów mózgu. W tym artykule przyjrzymy się bliżej przyczynom dyslipidemii oraz związkowi między cholesterolem a chorobami układu krążenia. Skupimy się również na znaczeniu profilaktyki i suplementacji, które mogą pomóc w walce z dyslipidemią.
Krótki przegląd artykułu:
- Czym jest cholesterol?
- Związek między cholesterolem a chorobami układu krążenia
- Przyczyny dyslipidemii
- Diagnostyka
- Jak sobie radzić z podwyższonym poziomem cholesterolu?
- Jakie suplementy mogą pomóc w przypadku dyslipidemii?
Czym jest cholesterol?
Cholesterol to substancja tłuszczowa naturalnie występująca w naszym organizmie. Jest to niezbędna cząsteczka występująca w każdej komórce , gdzie wchodzi w skład błon komórkowych. Cholesterol jest również prekursorem syntezy hormonów steroidowych – z cholesterolu powstają nie tylko hormony płciowe (np. testosteron, estrogeny i progesteron), ale także hormon stresu, kortyzol . Największa część cholesterolu jest wykorzystywana do syntezy kwasów żółciowych, które wspomagają trawienie tłuszczów . Wreszcie, witamina D powstaje w skórze z cholesterolu dzięki działaniu światła słonecznego.
Organizm produkuje większość cholesterolu, ale mniejsza jego część (około 20%) jest również dostarczana z pożywieniem. Zarówno cholesterol z pożywienia, jak i cholesterol syntetyzowany przez nasz organizm, jest transportowany w cząsteczkach lipoprotein (kompleksach lipidów i białek), które transportują tłuszcze nierozpuszczalne w osoczu krwi. Cztery główne grupy lipoprotein to:
- Chylomikrony powstają w jelicie cienkim i dostarczają bogate w energię tłuszcze z pożywienia do mięśni lub magazynują je w komórkach tłuszczowych. Chylomikrony transportują również cholesterol z jelit do wątroby.
- VLDL (lipoproteiny o bardzo małej gęstości) transportują lipidy — trójglicerydy, fosfolipidy i cholesterol — z wątroby do komórek tłuszczowych.
- LDL (lipoproteina o niskiej gęstości, powszechnie nazywana „złym cholesterolem”) transportuje cholesterol do tkanek. Może on również przedostawać się do ścian tętnic, przyczyniając się do miażdżycy i chorób układu krążenia. Cząsteczki LDL zawierają apolipoproteinę B100 (Apo-B100).
- HDL (lipoproteina o wysokiej gęstości, często nazywana „dobrym cholesterolem”) transportuje cholesterol z tkanek z powrotem do wątroby. Cholesterol w wątrobie może być ponownie przetwarzany i/lub wydalany z organizmu w postaci soli żółciowych. Transport cholesterolu z tkanek do wątroby nazywa się odwrotnym transportem cholesterolu. Cząsteczki HDL zawierają apolipoproteinę B (Apo-A).
Związek między cholesterolem a chorobami układu krążenia
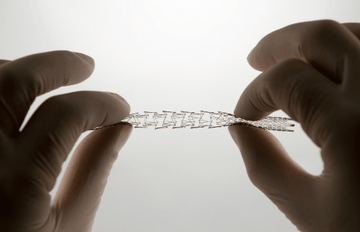
Synteza i wykorzystanie cholesterolu muszą być regulowane, aby zapobiec jego nadmiernemu gromadzeniu się i odkładaniu w organizmie . Nieprawidłowe odkładanie się cholesterolu i cząsteczek LDL w tętnicach wieńcowych jest znaczące. To odkładanie się może prowadzić do miażdżycy , która jest głównym czynnikiem przyczyniającym się do choroby wieńcowej. [1]
Należy jednak zauważyć, że procesy metaboliczne, takie jak utlenianie lub glikacja, odgrywają istotną rolę w tym, jak szkodliwe mogą być cząsteczki LDL dla komórek śródbłonka tętnic (i tym samym przyczyniają się do rozwoju miażdżycy). Wolne rodniki powodują uszkodzenia oksydacyjne cząsteczek LDL, a podczas glikacji cząsteczka cukru LDL zmienia swoją strukturę, tworząc glikowane cząsteczki LDL. Glikacja LDL , która jest zależna od stężenia cukru we krwi, może odgrywać bezpośrednią rolę w rozwoju miażdżycy i zwiększać podatność cząsteczki LDL na utlenianie. [2]
Podwyższony poziom LDL nie zagraża zatem bezpośrednio komórkom śródbłonka, ale oznacza, że dostępnych jest więcej cząsteczek LDL, które mogą zostać utlenione (lub w inny sposób zmodyfikowane), co z kolei może prowadzić do uszkodzenia naczyń krwionośnych.
Przyczyny dyslipidemii
Pierwotna dyslipidemia obejmuje genetycznie uwarunkowane zaburzenia metabolizmu lipidów , takie jak hipercholesterolemia rodzinna, hipertriacyloglicerolemia rodzinna czy hiperlipoproteinemia rodzinna. Zaburzenia te należą do najczęstszych chorób dziedzicznych i dotyczą około 1 na 500 osób. [3]
Problemem w hipercholesterolemii rodzinnej jest defekt receptora cholesterolu LDL w wątrobie. Normalnie komórka wątroby otrzymuje cholesterol LDL, który wiąże się z receptorem LDL, a wątroba otrzymuje sygnał do zaprzestania produkcji cholesterolu. W hipercholesterolemii rodzinnej uszkodzenie receptora LDL powoduje, że wątroba nie otrzymuje sygnału do zaprzestania produkcji cholesterolu. Uszkodzenie receptora LDL występuje również często w procesie starzenia się i w niektórych chorobach (zwłaszcza w cukrzycy).
Poziom cholesterolu ma tendencję do wzrostu wraz z wiekiem . Ponadto dieta bogata w tłuszcze nasycone i cholesterol zmniejsza liczbę receptorów LDL. Osłabia to również mechanizm sprzężenia zwrotnego, który nakazuje komórkom wątroby zmniejszenie syntezy cholesterolu. [3]
Wtórna dyslipidemia może być wynikiem innej choroby , takiej jak cukrzyca, dysfunkcja wątroby, dróg żółciowych, nerek lub tarczycy . Z tego powodu zaleca się, aby u pacjentów z dyslipidemią wykonywano również badania w celu sprawdzenia funkcji tarczycy. [4] Ponad 90% pacjentów z niedoczynnością tarczycy cierpi na dyslipidemię, ale tylko około 4% osób z dyslipidemią ma niedoczynność tarczycy. [5]
Dyslipidemia może również wynikać z czynników związanych ze stylem życia , takich jak nadmierne spożycie alkoholu, otyłość, a także choroby zakaźne . W przypadku infekcji bakteryjnych lub wirusowych stężenie trójglicerydów zwykle wzrasta. Dlatego badanie profilu lipidowego nie jest wskazane wkrótce po chorobie zakaźnej. Zaleca się wykonanie lipidogramu około trzech tygodni po łagodniejszej chorobie i około trzech miesięcy po cięższej chorobie. [6]
Diagnostyka
Dyslipidemię często wykrywa się podczas badania profilaktycznego , na podstawie wyników badań krwi, podczas którego wykonuje się lipidogram pacjenta. Zaleca się regularne monitorowanie profilu lipidowego u pacjentów z historią rodzinną dziedzicznych zaburzeń metabolizmu lipidów oraz u pacjentów z podwyższonym ryzykiem chorób układu krążenia. Podstawowym badaniem jest oznaczenie stężenia cholesterolu całkowitego, LDL i HDL oraz trójglicerydów.
Inne markery dyslipidemii również powinny być badane. Jednym z nich jest na przykład apolipoproteina B. Apolipoproteiny to białkowe składniki lipoprotein, a Apo-B jest markerem liczby wszystkich miażdżycogennych cząsteczek lipoprotein w krążeniu. Wiele badań przeprowadzonych w niedawnej przeszłości wykazało, że podwyższony poziom Apo-B jest lepszym predyktorem ryzyka chorób sercowo-naczyniowych niż tradycyjne markery wymienione powyżej. [7] Dlatego wiele grup ekspertów zaleca oznaczanie Apo-B w celu oceny ryzyka sercowo-naczyniowego. [11]
Innym pomocnym markerem jest białko C-reaktywne (CRP) produkowane przez wątrobę, które ocenia stan zapalny lub chorobę zakaźną. Rozwój miażdżycy jest związany ze stanem zapalnym w ścianach naczyń, dlatego poziom hs-CRP może wskazywać na ryzyko rozwoju choroby sercowo-naczyniowej. Wykazano, że CRP koreluje z zaawansowaniem miażdżycy, a podwyższony poziom trójglicerydów i BMI są ściśle związane z wysokim poziomem CRP u pacjentów z dyslipidemią. [8]
Jak sobie radzić z podwyższonym poziomem cholesterolu?
Podstawą leczenia dyslipidemii są działania niefarmakologiczne . Należą do nich w szczególności: regularna aktywność fizyczna, optymalizacja masy ciała (BMI 20–25 kg/m², obwód talii <94 cm u mężczyzn i <80 cm u kobiet), rzucenie palenia, ograniczenie spożycia alkoholu oraz zapobieganie lub kompensacja stresu . Oczywiście, modyfikacja diety, z naciskiem na dietę śródziemnomorską, jest również kluczowym czynnikiem w leczeniu dyslipidemii.
Jakie suplementy mogą pomóc w przypadku dyslipidemii?
Można zalecić kilka strategii wspomagających leczenie dyslipidemii. Jednak zaniedbanie niezbędnych czynników żywieniowych może prowadzić do podwyższonego poziomu lipidów we krwi . Dlatego wybraliśmy z naszej oferty następujące kluczowe suplementy, na których skupimy się w przypadku dyslipidemii.
Kwasy tłuszczowe omega-3
Zwiększone spożycie kwasów tłuszczowych omega-3 działa przeciwzapalnie i pomaga utrzymać zdrową równowagę między kwasami tłuszczowymi omega-3 i omega-6. Brak równowagi między kwasami tłuszczowymi omega-3 i omega-6 wiąże się z różnymi chorobami zapalnymi, w tym chorobami układu krążenia. Kwasy tłuszczowe omega-3 mają również korzystny wpływ na metabolizm lipidów i cholesterolu . Zapewnienie odpowiedniej ilości kwasów tłuszczowych omega-3 wiąże się zatem ze zmniejszonym ryzykiem chorób układu krążenia.
Wskaźnik Omega-3 to użyteczny wskaźnik określający ilość kwasów tłuszczowych omega-3 w organizmie. Jest on wykorzystywany jako niezależny czynnik ryzyka chorób układu krążenia i stanowi cenne narzędzie oceny stanu zdrowia.
Magnez
Magnez jest jednym z często brakujących minerałów w organizmie człowieka. Pierwiastek ten jest niezbędny do wszystkich reakcji, w których powstaje energia, a jego niedobór objawia się na przykład zmęczeniem. Magnez jest również nadmiernie niedoborowany w okresach wzmożonego stresu (zarówno psychicznego, jak i fizycznego). Jednak magnez reguluje również enzym reduktazę HMG-CoA, który wpływa na metabolizm cholesterolu (ten sam enzym, na który oddziałują statyny). Zatem niedobór magnezu może przyczyniać się do podwyższonego poziomu cholesterolu i negatywnie wpływać na powstawanie blaszek miażdżycowych.
Witamina E
Witamina E jest ważnym przeciwutleniaczem, poprawia wrażliwość komórek na insulinę oraz zmniejsza uszkodzenia oksydacyjne cząsteczek LDL i nadmierną agregację płytek krwi. Witamina E to nazwa grupy ośmiu form związków – czterech tokoferoli (alfa, beta, gamma i delta) oraz czterech tokotrienoli (alfa, beta, gamma i delta). Pełne spektrum witaminy E i tokotrienoli zawarte w ProLife ma szereg korzyści zdrowotnych w porównaniu z samym alfa-tokoferolem . Tokotrienole blokują enzym reduktazę HMG-CoA, hamując w ten sposób produkcję cholesterolu w organizmie i pomagając obniżyć jego poziom. [9]
Witamina D
Badania wykazały, że niedobór witaminy D wiąże się ze zwiększonym ryzykiem chorób układu krążenia i innymi czynnikami ryzyka, takimi jak dyslipidemia, nadciśnienie i cukrzyca. [10] Każda komórka w organizmie ma receptor witaminy D, co pokazuje jej znaczenie.
Zaleca się zmierzenie poziomu witaminy D i dostosowanie suplementacji na podstawie uzyskanych wyników. Możesz skorzystać z naszego domowego zestawu do pomiaru poziomu witaminy D, aby sprawdzić, czy masz wystarczającą ilość tej kluczowej witaminy, bez konieczności udania się do punktu diagnostycznego.

Źródła:
[1] Cholesterol: synteza, metabolizm i regulacja, strona biochemii medycznej
(https://themedicalbiochemistrypage.org/cholesterol-synthesis-metabolism-and-regulation/)
[2] Fournet M, Bonté F, Desmoulière A. Uszkodzenia glikacji: możliwe źródło głównych zaburzeń patofizjologicznych i starzenia się. Aging Dis. 2018 1 października;9(5):880-900. doi: 10.14336/AD.2017.1121. PMID: 30271665; PMCID: PMC6147582.
[3] Pizzorno Joseph E., Murray Michael T., Podręcznik medycyny naturalnej, zestaw 2 tomów. Wydanie piąte, Elsevier. 2021
[4] Rizos CV, Elisaf MS, Liberopoulos EN. Wpływ dysfunkcji tarczycy na profil lipidowy. Open Cardiovasc Med J. 2011;5:76-84. doi: 10.2174/1874192401105010076. Epub 24 lutego 2011. PMID: 21660244; PMCID: PMC3109527.
[5] Šatný M., Vrablík, M. Sekundární dyslipidemie – přehled pro praktické lékaře. (https://www.medicinapropraxi.cz/pdfs/med/2019/05/11.pdf)
[6] Soška V., Sekundární dyslipidemie a jejich léčba. (https://www.casopisvnitrnilekarstvi.cz/pdfs/vnl/2007/04/14.pdf)
[7] Feingold KR. Wprowadzenie do lipidów i lipoprotein. [Aktualizacja: 19 stycznia 2021]. W: Feingold KR, Anawalt B, Blackman MR i in., red. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Dostępne na stronie: https://www.ncbi.nlm.nih.gov/books/NBK305896/
[8] Swastini DA, Wiryanthini IAD, Ariastuti NLP, Muliantara A. Prognozowanie miażdżycy przy użyciu białka C-reaktywnego o wysokiej czułości (hs-CRP) i powiązany czynnik ryzyka u pacjentów z dyslipidemią. Otwarty dostęp Maced J Med Sci. 2019 14 listopada; 7(22):3887-3890. doi: 10.3889/oamjms.2019.526. PMID: 32127998; PMCID: PMC7048367.
[9] Baliarsingh S, Beg ZH, Ahmad J. Wpływ terapeutyczny tokotrienoli u pacjentów z cukrzycą typu 2 i hiperlipidemią. Miażdżyca. Październik 2005;182(2):367-74. doi: 10.1016/j.atherosclerosis.2005.02.020. Epub 20 kwietnia 2005. PMID: 16159610.
[10] Kim MR, Jeong SJ. Związek między poziomem witaminy D a profilem lipidowym u dzieci nieotyłych. Metabolity. 2019 30 czerwca; 9(7):125. doi: 10.3390/metabo9070125. PMID: 31262034; PMCID: PMC6680594.
[11] Contois JH, McConnell JP, Sethi AA, Csako G, Devaraj S, Hoefner DM, Warnick GR; Grupa robocza ds. najlepszych praktyk Wydziału Lipoprotein i Chorób Naczyniowych AACC. Apolipoproteina B i ryzyko chorób sercowo-naczyniowych: oświadczenie stanowiska Grupy roboczej ds. najlepszych praktyk Wydziału Lipoprotein i Chorób Naczyniowych AACC. Clin Chem. 2009 marzec;55(3):407-19. doi: 10.1373/clinchem.2008.118356. Epub 2009 styczeń 23. PMID: 19168552.